Recovery Capital Conference of Canada

By Joe C.
“Having been at addiction-oriented events across the USA and Canada I have found that we are creating addiction experts; that’s great. But I go to these things and I ask myself, ‘When is anyone ever going to talk about recovery?’” These are the thoughts of the Director of Community Development for the Last Door Recovery Centre in New Westminster British Columbia, Giuseppe Ganchi.
In the Vancouver BC listening area or anywhere you have internet, Thursdays from noon to 1 PM, along with co-hosts Frances and Darren, Giuseppe had been leading by example on a radio show called, Talk Recovery Radio.
Giuseppe chaired the 2018 Recovery Capital Conference of Canada which I attended at downtown Toronto’s The Carlu Centre, September 13th and 14th. A somewhat similar program was presented in Vancouver’s lower mainland earlier in the month.
With a team of like-minded west-coast individuals, Giuseppe and company put their love and service where their mouth was and created a venue to bring people together to talk about recovery. Now in the second year, with a Toronto partner in Bellwood and Edgewood Health Services, there are discussions about replicating this formula in Calgary Alberta very soon, too.
Here’s a run down about some of the presentations, chatter over coffee and discussions among old and new friends…
The Portugal model is best known for their de-criminalization of drug use. Addiction as a public health problem and not a criminal problem is only part of the Portugal Model. Recovery Capital’s opening speaker, Dr. Manuel Cardoso, Deputy General – Director of SICAD Decriminalization and Portugal Public Health Policy – explained that dissuasion is the Portugal model. First, decriminalization helps destigmatize addiction, but Portugal is committed to making treatment accessible to those in need.
Friday afternoon the conference was closed out with a case study of Philadelphia’s Public Health Approach to Promote Recovery, presented by Arthur C. Evans, Jr., PhD, Chief Executive Officer and Executive Vice President, American Psychological Association. “I hear a lot of talk around here about the best form of treatment. We aren’t debating about harm reduction vs. abstinence-based treatment where I come from; you want to know why?” Dr. Evans asked, “Because our priority is long-term recovery and how people get their business. Everyone has a right to dignity and choice.”
Between now and the end of your coffee (or other refreshment), I will attempt to offer some breadth of discussion about Recovery Capital discussion that took place between these two book-ends of Portugal and Philadelphia.
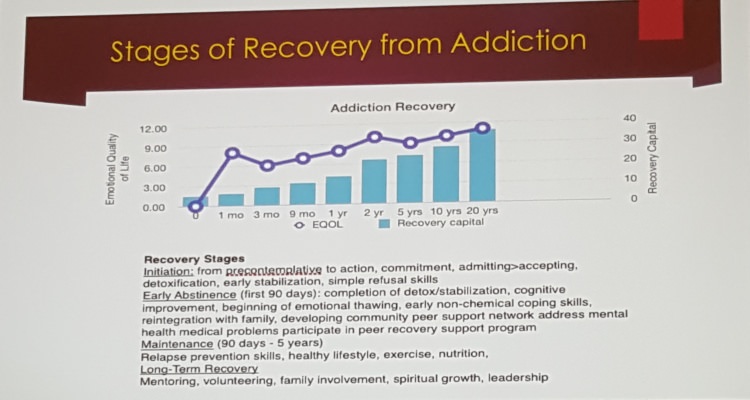
One of the slides shared at the Recovery Capital Conference: The Stages of Recovery.
A panel of mostly lived-experience, Building Resilience with Recovery Capital was moderated by Ann Dowsett Johnston, journalist/author of Drink: The Intimate Relationship Between Women and Alcohol and offered contributions from Habib Hass, a PhD candidate, Tristan Johnson, Alumni Outreach Coordinator from Bellwood Health Services and Betty-Lou Kristy, director of Centre for Innovation in Peer Support. The takeaway is that both addiction and recovery are as individual as each of our fingerprints. Culture, economics and our own personality will inform both our barriers to recovery and our recovery lifestyle.
A persistent myth is that we have no scientific data about 12-Step recovery, in-patient or out-patient treatment. Critics rail that addiction/recovery is a multibillion-dollar industry founded on dodgy, anecdotal practices and unproven approaches. While wanting to get good value for time and money spent on recovery is prudent, the idea that recovery is mysterious is an outdated notion. Over the last 20 or more years a great deal of research and science has gone into better understanding addiction and recovery.
Dr. Julian M. Somers of Simon Fraser University presented on, Recovery Capital: When Wealth and Poverty Have the Same Price. Science debunks the notion that treating addiction is unaffordable or expensive. From providing housing to the homeless to giving care to those with substance-use disorder, the data shows that we, as a society, save money when we invest in recovery – the results are a financial gain, not a cost. In the same way providing housing costs society less than health-care costs for the homeless, treating addiction costs less than the havoc we wreak on family and society when we are in our addiction. If you’re not up to date, over the past 10 years a series of studies in British Columbia have involved people experiencing complex addictions. This research has used a variety of methods: economic analyses; cohort studies; randomized controlled trials; qualitative interviews; and comparative outcome studies. Many of these studies have focused on integrated multi-agency interventions.
Some of my preconceived ideas were born of old data and Julian Somers dispelled some of this for me.
Also from and for the fact-file, Dr. J Kelly, Harvard, Professor of Psychiatry in Addiction Medicine at Harvard University reviewed the last 50 years of addiction law including the mid-1980s Anti-Drug Abuse Act and the more recent Comprehensive Addiction & Recovery Act of 2016. And as for recovery capital, a 2018 Alcoholism: Clinical and Experimental Research revealed Recovery Indices by Years since Problem Resolution. Psychological distress dissipates in recovery. On the upswing is Quality of Life, Happiness and Self Esteem. In a nutshell, there’s recovery capital by the numbers. Twelve Step-Facilitation nay-sayers argue that the model is unproven and ineffective. Dr. Kelly revealed that compared to other theoretical orientation treatments such as enhanced motivational interviewing, cognitive behavioral therapy and individual psychotherapy, going to meetings, getting a sponsor, working the steps was as effective or more effective and considerably less costly in terms of the financial burden on families, companies and/or society. One two-year longitudinal study shows 12-step treated patients were more likely to abstain compared to CBT with a $8,000 per patient savings. This isn’t anti-CBT or anti-anything. The point is that much of the “AA is unproven” argument is outdated.
Key contributors to the Recovery Capital Conference came from the rank and file of the Centre for Substance Use and Addiction. Maybe it was a widely shared experience that NA or AA was the last house on the block for people like me who struggle with substance use. That might have been the truth or close to it, back in the day. But as I look over my shoulder now, besides that 1930s house at the end of the block, I see an entire sub-division of agencies and resources and know-how when it comes to addiction and mental health. CCSA wasn’t around when I got here. Today, they provide national guidance to decision makers by harnessing the power of research, curating knowledge and bringing together diverse perspectives.
Building Recovery Capital: Mining, Defining and Utilizing was a presentation that teamed up Gord Garner. Executive Director, Community Addictions Peer Support Association with Rebecca Jesseman, Director of Policy CCSA to combine data and lived-experience. First, the data. Here’s some of the facts CCSA has mined about alcohol and other drug use in Canada:
Among survey respondents who report “monthly or more often risky alcohol consumption, over 50% aged 19-24 engage in risky alcohol consumption. Over 40% of 25-34-year-olds, over 30% of both underage (drinking age in Canada is 18 or 19 depending on the Provence) and 35-44-year-olds, 25% of 55 to 64-year-olds and 10% of 65+ respondents.
In another study, more males than females engage in risky alcohol consumption. At risk are 15% of females and 30% of males. Fifty-four percent of teens have tried illicit drugs and half of under-19s report using/trying cannabis.
To cheer us up, in 2017 CCSA researched and reported on, Life in Recovery from Addiction in Canada. Of Canadians in recovery, 72% report quality of life as being either very good or excellent. That’s not what we thought when we walked through the doors, was it? Only 2% reported a poor quality of life. In a table resources utilized from 12-Step to non-12-Step peer-to-peer, both in-and-out-patient treatment, counseling and other medical and psychological therapies, reaction showed many paths lead to and maintain recovery. Most people use now or have used multiple aids to find recovery. It isn’t uncommon for respondents to list over five different practices or interventions that contributed to their recovery. Canadian findings were compared to Australia, USA and the UK.
So that’s the data, now how can data influence policy and affect change? “There’s a story behind the numbers,” Rebecca Jesseman (CCSA) told us. “If you don’t tell the stories behind the numbers, it’s hard to bring the numbers to life. When you’re trying to influence policy, you give them the story and make the story real.”
Teamed with Community Addictions Peer Support Association, executive director, Gord Garner, Rebecca Jesseman gave an effective and emotional presentation of scientific data and lived-experience; facts with feeling!
In a Recovery Coaching Workshop, Dr. Ray Baker, MD, Consultant in Recovery Medicine, made a compelling case that recovery-coaching could be the most important element in recovery-oriented care. To be a coach requires a unique set of competencies delivered by trained paraprofessionals. This idea isn’t a panacea. It’s unregulated and under-appreciated. Dr. Baker’s session reviewed required attitudes, knowledge and skills. A coach is not a counselor or a doctor, any more than your skating, football or track and field coach is.
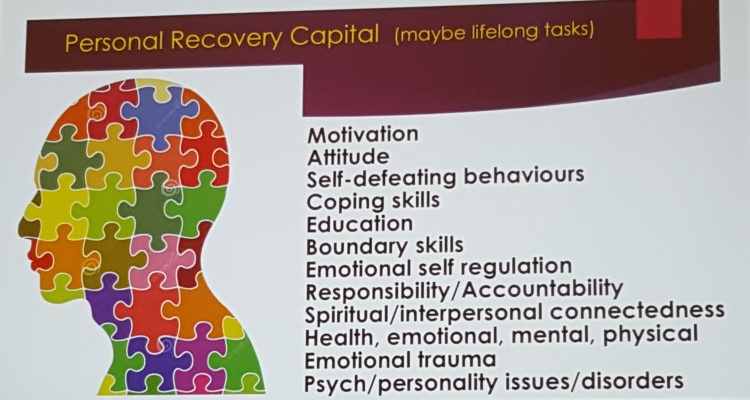
Another shared slide: Some of the assets that are part of our recovery capital.
Workplace Wellness was covered in a two-part session by, Christine Burych, President of Starling Brook Leadership. What generation do you think suffers the most work-related anxiety (that leads to work-place health issues)? Is it the Silent Generation, Baby Boomers, Gen-X or Millennials? It’s Millennials; I didn’t know that.
Yoga – by example – was brought to us by Evonne Sullivan with mindfulness and meditation for mental health and addiction recovery breaks and practices between sessions. Evonne Sullivan works with a variety of organizations such as the Centre for Addiction and Mental Health (CAMH), offering services in mood and anxiety, trauma, concurrent disorders and medical withdrawal units.
Hamish White and Dr. Michele Pole spent an hour on, An Integrated Treatment Model for Addiction and Trauma/PTSD. Here’s something I didn’t know – “trauma informed” doesn’t mean your healthcare worker or treatment centre is trained to help me deal with an underlying mental/emotional disorder. “Informed” doesn’t always mean, “qualified.” Chalk that up for one more, “I did not know that,” helpful tidbit from the two-day session.
It wasn’t possible to take in everything I found interesting. There was a lot of talk about the potential health-issues of legalized cannabis use. There were other sessions that, if it was a four-day conference, I could have sat in on. I am left to hope that some it sunk in. There wasn’t much time or much of an urge to check my Twitter or Facebook; interesting and stimulating presentations just kept coming. There were great networking opportunities, too.
What impressed me most about the Recovery Capital Conference was hearing talks and discussions for two full days about evidence-based approaches to substance use disorder. We checked off where we’re at today and candidly shared on what needs to be done next.
Here is a great link about the conference: Rebellion Dogs 38 Recovery Capital 2018.
Want to read this article again, or later today? Perhaps it’s one you would like to share with a friend. For a PDF just click here: Recovery Capital Conference of Canada.







Very helpful Joe!
I sure wish I could attend these kinds of events so I am greatful for such a good report or summary of the key items of value.
Well done!
Joe, thanks, I think it is a really good development that we are listening to the professionals in the field. I have often had the impression that co-operation with the professional community has consisted in not much more than AA telling them what to do. I’m glad we’re listening now.
And recovery capital is an important concept.
Yes, thanks much for your summary, Joe – I’m so glad you were there.
I love it when science/stats and experiential merge.
Here’s hoping for more of these opportunities in Canada.
Thanks Joe for your fine review of the sessions you attended. I was especially interested in Harvard Professor Dr. J Kelly’s research. I know you have always been a strong adherent of the reality that there are many paths to recovery and all are cause for celebration. So when you report that —“One two-year longitudinal study shows 12-step treated patients were more likely to abstain compared to CBT with a $8,000 per patient savings. This isn’t anti-CBT or anti-anything. The point is that much of the ‘AA is unproven’ argument is outdated.” — you are not AA thumping in any way but simply suggesting that decades old scepticism regarding AA’s efficacy must itself become the object of sceptical inquiry.
Excellent report!
Why, with all the new information available, in AA, do we only use an 80 year old book?
I feel your frustration, Marty.
AA as a big-book-culture is a time and place issue. So the “we” has to be defined because not all AA meetings run just like all the others, as you know. Personal Example: I got sober in a non-Big Book climate. It wasn’t anti-Big Book or anti-anything but the Montreal and area AA of the mid-1970s was mostly speaker meetings and discussion meetings. If we read, it was most likely from Grapevine, Came to Believe or Living Sober which was new to AA in 1973. Living Sober is a good example. While Alcoholics Anonymous (the book) was descriptive – not prescriptive when written. The Steps aren’t instructions and the Traditions aren’t rules. They are descriptions of our experience the best we could do, speaking in the “we” authorship. Perhaps that’s why more pages are devoted to personal stories – “I” authorship which is more how one AA talks to another. I know that some AAs refer to our first book as instructional and treat the Traditions as a means of policing others but I don’t think this was the original intent.
So the Big Book was three or four years of our collective wisdom. While it was debated if writing it down was a good idea, I think most agree that it was a good idea. Then Living Sober was our 40-years of collective experience (written by one Barry L but drawing upon the wisdom of the rooms). So in 1976, where I got sober, it made sense to draw on a greater breadth of experience – Living Sober.
I later moved to Calgary for five years and while meetings were quite different in a smaller, Western city, I don’t remember any Big Book meetings. It wasn’t until I came to Toronto, nine 1/2 years sober that I found myself in a Big Book culture and it wasn’t the whole city but reading from the book was common place. I didn’t own one, I hadn’t read it. It wasn’t until an AA gave me Pass It On for my 10th anniversary and I read that, that I got interested in AA history and I read the Big Book to better understand our history. I did the Steps before I read it, I got sober before I read it so my relationship to the book is very different to those who recognize it as the cornerstone to their salvation.
Today, my AA group doesn’t read the Big Book. Many of us do and some of us attend Big Book meetings but our group relies on lived-experience, the AA oral tradition of one alcoholic talking to another, or many. That’s how AA worked before there was a book, I’m thinking.
At a recent meeting the chair read from a web-news page about addiction and recovery and that informed our group discussion for the hour. Of course, anyone could talk about whatever they liked.
I know what you mean about the “AA as a whole” we and regardless of it being a perception or reality, that “we” may feel AA is the book and the book is AA – you don’t have one without the other. But I think the “Group autonomy” we is bigger than the “AA as a whole” we. It’s more practical and less abstract.
I tend to get lofty in my “what’s good for AA” chatter and my mind is on what GSO should do but AA is my group, my group’s business meeting and how I, if I wish to, greet newcomers to AA. I try now to focus my “making AA better” efforts now about 75% in my engagement with my group and local AAs and 25% on the lobbying AA with my “adapt or perish” rants.
Many people see both correlation and causality with reading the Big Book and getting sober. I can’t pretend that is my experience. But now, I am less inclined to argue that it isn’t their reality, either. I want to be free to believe as I wish so I try to offer the same courtesy. I’m glad they get what they need from reading 164 pages over and over and they have meeting that support this ritual. I tried it a couple of times and it felt like repetitive strain disorder. Of course that doesn’t make them or me right or more right than the other.
While Marty got me rambling, I appreciate everyone’s insights. I hope these types of gatherings become more common and more affordable and more of us get to participate in them.