Addiction and Suffering – Gabor Maté
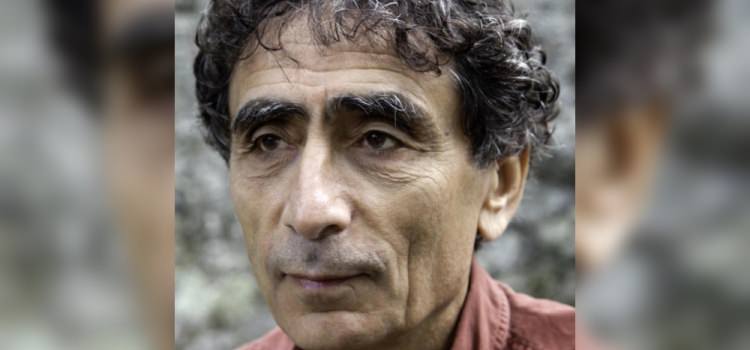
Dr. Gabor Maté specializes in the study and treatment of addiction and trauma. He is well known for his firmly held belief in the connection between mind and body health. Dr. Maté’s bestselling books include the award-winning In the Realm of Hungry Ghosts: Close Encounters with Addiction. Rather than offering quick-fix solutions to complex issues, Dr. Maté weaves together scientific research, case histories and his own insights to present a broad perspective.
For over a decade, Dr. Maté worked in Vancouver’s Downtown Eastside with patients challenged by drug addiction, mental illness and HIV, including a stint at North America’s only supervised injection site. Beyond his work with addicts, he has over 20 years of family practice and palliative care experience. Dr. Maté regularly speaks to health professionals and lay audiences across North America. He has received the Hubert Evans Prize for Literary Non-Fiction and the 2012 Martin Luther King, Jr. Humanitarian Award from Mothers Against Teen Violence.
By John Lavitt
Originally published on January 6, 2016 on The Fix.
You have said that you believe that, “many doctors seem to have forgotten what was once a commonplace assumption, that emotions are deeply implicated in both the development of illness, addictions and disorders, and in their healing.” When I got sober at Beit T’Shuvah, the Jewish rehab in Los Angeles, Rabbi Mark Borovitz often told us to forget our feelings and focus on our actions. A common saying in 12-step groups is that you have to act yourself into right thinking. Can you also act yourself into right emotion?
Can you act yourself into the right emotion? Let me put it this way, John; the question does not interest me. What interests me is for people to really know where they are coming from and where their actions come from. People can act the right way, but that doesn’t mean they are being the right way. You can’t force emotions; you really have to know what they are. For me, the important question is, what are the actual emotions underneath the action that are driving my behavior and where do those emotions come from? For me, it’s not a question of acting into the right emotion. It’s a question of understanding what are the source emotions from which we are acting. That is the really important question.
I completely appreciate the 12 steps, and I talk about them in my book where I have an appendix on them. I think where they fail or where they miss something is when they focus on action while tending not to look at the underlying emotions and the experiences that underlie those emotions. You can go to 12-step groups for a long time and never find out how traumatized you were. That’s where the missing piece is and has been for a long time.
The patients that I worked with – I’m talking about hardcore, street level drug users, people injecting cocaine and heroin and so on – not a single one of them ever came to me and said, “Doc, I was traumatized, and I’m using that as an excuse to do drugs.” They didn’t know they were traumatized. No doctor had ever pointed it out to them. They thought they were just fuck-ups. They thought they were just bad people. They thought they were just addicts. They didn’t realize that they were using the addiction to soothe a deep pain that was rooted in trauma. In all cases of addiction that I have seen, there’s deep pain that comes out of trauma. The addiction is the person’s unconscious attempt to escape from the pain.
That’s not just my personal opinion. It’s also what large-scale studies show. In large population studies, you find that extreme trauma, whether in a population like the Native Indian population in your country or the Aboriginal population in Australia or the Native population in my country with the loss of land and the violence and the forced abduction of their children who were brought up for a hundred years in residential schools away from their families where they were sexually abused, generation after generation, there’s a huge statistical and causative link between that trauma and the addiction. That’s not a theory. It’s just reality.
And it’s not only that. We also know that the brain itself, the human brain itself, is shaped by the environment. The brain is not purely genetically programmed. Brain development occurs in reaction to the environment. The necessary conditions for healthy brain development are healthy relationships with responsive parents. When the parenting environment becomes distorted or hostile and abusive, you’re actually distorting people’s brain development. This means they are going to be more likely to want to use substances to feel better in their brain in order to achieve a different state of the brain.
Whether we are talking about the emotional pain and the shame that’s at the heart of addiction or whether we are looking at the brain physiology of addiction, which is very much influenced by childhood experiences, we are looking at the impact of trauma.
To go back to the original quote about doctors, if we actually understood that all behaviors are for the most part coping mechanisms for emotions that we are not able to deal with, then the focus could shift not just to changing behaviors, but actually understanding the emotions that underlie them. That’s what I think is missing from medical practice. Whether it’s addictions or whatever it is, we are not seeing what’s driving it and what’s underneath it. That’s why I said the question did not interest me. I’m trying to turn your questions around on its head or I’m trying to put it back on its feet. Let’s put it that way.
In an article about the death of Robin Williams, you wrote, “While there may be genetic predispositions toward depression and addiction, a predisposition is not the same as a predetermination.” If a family knows that their child has a predisposition toward either addiction or depression, or both given the commonality of co-occurring disorders, what can they do to help ensure their child lives a healthy, happy and productive life?
Let me turn that question around again. Does it matter what you know? Don’t you want to give them a childhood in which they are loved, in which they are respected, regardless? You want to give them a childhood where they are accepted for who they are, where they are celebrated for who they are, where they can explore the world under guidance but with freedom, where they can be themselves and be happy being themselves. There is no difference in how you should want to parent one child as opposed to another child.
This is how we want to parent children, and it doesn’t matter what predispositions a child has, if they get these conditions of love and respect in their childhood, they’ll never be addicted, they’ll never get depressed and they’ll never be anxious – not in terms of the medical diagnosis of those conditions.
Any person might experience anxiety at some time or sadness. I’m not talking about that, but in terms of the so-called illnesses, they will never happen. It doesn’t matter what we know about our children’s predispositions. The question is, what kind of childhood do human beings require to be healthy, self-realized creatures? Look at all of the characteristics that I listed.
The question is, why the disease focus? Your question is very disease-focused. How do I prevent a disease? That’s not the right question. That’s already coming out of fear. You don’t want to parent out of fear. The right question is what does a human being need, any human being.
Explaining the disease-prone personality, you said, “No personality causes disease. So there’s no cancer personality. However, there are some common traits that, if they are present in exaggerated degrees, will make you more predisposed to the disease. They don’t cause it, but make you more likely to get it because they increase the amount of physiological stress you’ve got inside you… Stress is the thing that leads to disease or leads to conditions for it, but certain personalities are more prone to this stress.”
Such a concept is somewhat alien to mainstream medicine. Do you believe it can be proven? Is the idea of the disease-prone personality a philosophical supposition or a medical reality?
This is not really controversial at all because it’s a medical reality. It’s only controversial because most doctors don’t know about it. If you look at studies of patients with malignant melanomas, for example, there is no absolute cancer personality, and you explained this idea very well. But there is no one type of personality that means you are going to get this disease. That’s not going to happen. You can’t say that there’s a disease personality. But there are definitely disease prone personalities; certain personality traits that make a person much more likely to have a disease than people who don’t have that type of personality. There’s no question about that.
It’s important to note that this tendency was discovered in relationship to malignant melanoma. People who developed malignant melanomas often tended to be people who didn’t express emotion in a healthy way and who suppressed or repressed their anger. Those are risk factors for illness. We know that. The repression of anger suppresses the immune system as opposed to healthy expressions of anger. It’s not a question of philosophy.
I was a physician for 33 years, and I didn’t begin with any of these assumptions. Nobody had told me about this. I just kept noticing, particularly when I worked in palliative care for seven years. We looked after terminally ill people, people who were dying of cancer, and I kept noticing and kept noticing and kept noticing that these people with auto-immune disease or with cancer typically had very tough childhoods where they survived by repressing their emotions, and that suppression of emotion was tied to their development of disease.
But I wasn’t the first one to notice this connection. It turns out that many doctors had remarked on this before. It had been noticed in ancient times, in Roman times. We are talking about doctors who go beyond just the body and are willing to look at the whole personality. They can’t help but notice that certain emotional patterns, certain personality traits make it more likely that you are going to get that disease. It’s an observation, and whenever it’s been studied, it’s been shown to be the case. There have been many studies, and I outline many of those studies in my book, When the Body Says No, Exploring the Stress-Disease Connection. I am talking about clinical observations backed up by studies.
In an article about actor Cory Monteith’s overdose and celebrity death in general, you wrote, “In our celebrity culture only the demise of a famous person attracts press attention to what is a daily human tragedy across North America and the world. Many other human beings succumb to drugs, an entirely preventable carnage that almost completely eludes public notice.” How can celebrity drug-fueled deaths be used by the mainstream media to raise awareness about addiction? Is such a moment possible in today’s opioid abuse epidemic?
A recent article in The New York Times revealed how it’s now been shown that the life expectancy of middle-class whites is going down. More and more are dying before their time, and much of that decrease in longevity is being caused by drug overdoses, and the effects of drugs and alcohol use on this population. Although it’s a serious problem, more awareness seems to come about the problem only when a celebrity dies. Although the drug problem is getting more and more attention just because it’s killing so many more people, a celebrity death results in a sudden infusion of attention.
However, nobody’s linking that to trauma. Like Dr. Oz will have a show on addiction because it’s a big deal now to talk about addiction, but trauma won’t be mentioned. Society and the medical profession are in denial of the role of trauma in this problem. As long as we are in denial of trauma, we’re never going to understand addiction. The “aha” moment that needs to occur is not that we recognize how bad addictions are, but that addictions are about an escape from trauma, and this society traumatizes people. Life in this society means that a lot of people are going to become traumatized. That’s the “aha” moment that hasn’t happened yet.
I believe people are actually looking for the truth. In terms of the mainstream media, that hasn’t happened. The “aha” moment where the connection between addiction and trauma is recognized is what is needed. It doesn’t have to happen in relation to me and my work – I’d love it if it was – but just in general, it needs to happen. We just keep talking about this bad problem of addiction, but we don’t want to look at what it’s really all about.
You have written about The Power of Negative Thinking, and the dangers of embracing an absolute positivity. You pointed out in a recent interview that, “Not having negative thoughts is not allowing reality to intrude on your perception of the world. You never see how things are. You have to always maintain a sunny, falsely rosy view of the world so that you can’t see what doesn’t work. Lots of studies show that people who are sunny and positive die quicker of their disease. If you’re a woman with breast cancer and you’re a positive thinker, you’re guaranteed to die much quicker.”
How have you come to such a conclusion that goes against the mainstream emphasis on the power of positive thinking? What is the relationship between the power of negative thinking and cathartic experience? Is opening the door to negativity an honest perception of the reality of the world, a healthy way to purge the trauma from your own mind and soul?
When I talk about negative thinking, you must understand that I’m being tongue-in-cheek. I don’t want people to think negatively, but I put that idea out there as a way of counteracting this relentless cheerful positivity that’s often given as the answer to the world’s problems. To my mind, we don’t need positive thinking or negative thinking; we need thinking. Thinking means you don’t load your point of view with either a priori negative or positive vibes. Rather, you are simply willing to look at what is. The positive thinkers are in full denial of reality.
Barbara Enright wrote a book called Bright-Sided: How Positive Thinking Is Undermining America. I am very much with her. When I talk about negative thinking, I’m talking about the willingness to look at reality however it is. It is not a question of whether it’s positive or negative, but rather a question of looking honestly at it.
In palliative care, in which I worked for seven years looking after terminally ill people, I had so many people say to me, “Doc, I don’t know what I’m doing here. I’ve never had a negative thought in my whole life.” And I thought to myself, that’s why you’re here. You were in denial of reality. You suffered so much as a child that the only way to survive was to suppress your awareness of pain and suppress your awareness of your own suffering. You coped in ways that ended up making you more stressed because you took on too much because you were not willing to look at what it was costing you. That’s why I argue that relentless positive thinking is actually pathological. That doesn’t mean I want people to think negatively. I just want people to think, which to me means a willingness to face reality exactly the way it is.
In a letter criticizing Canada’s Health Minister Rona Ambrose’s voiding of a harm reduction policy where doctors could prescribe heroin to a very select and limited number of clients, you wrote, “There has been no sign that you or your government pay the least attention to scientific data in formulating drug policies.” If you had the power to change the way a government dealt with addiction and treatment, what policies and regulations would you set into place?
First of all, I am pleased to say that Ms. Ambrose is no longer Canada’s health minister. Her government was defeated recently, and many people ended up breathing a sigh of relief over that one. This government was completely hostile to vulnerable people, including Native people and including addicts. She had tried to close a facility where I worked that was America’s only supervised injection site where people were actually given clean needles and sterile water to inject their drugs with. They wanted to shut it down even though it saved lives, even though it saved healthcare costs, even though it reduced crime. Despite all these things, they still wanted to shut it down.
What we need is the very opposite. What we need is a policy that recognizes that addiction is not a choice that anybody makes, that addiction is actually a response to suffering, that it’s a response to childhood suffering. The addict needs not hostility and punishment, but compassion and understanding. What we need is not just changes in behavior on the part of the addict or medical treatments only, but we actually need an approach that is compassionate; that means we stop punishing people for trying to escape from their suffering. You stop doing that; you don’t make them suffer more. That’s not going to help them give up their addiction.
Jailing, as you have in your country, many hundreds of thousands of people, millions of people, that’s not going to stop addiction. It’s just going to make it worse. Addiction is a response to suffering. You’re not going to make people give up addiction by making them suffer more. If people only got a basic understanding of the link between trauma and addiction, if they looked at the science of brain development and of childhood development, if they are willing to look at the statistical correlation between childhood adversity and addiction, if they are willing to treat people like human beings who suffered and whose addiction is a response to suffering, then we’ll have some decent treatment programs. If all the money that now goes into punitive or useless approaches would now go into compassionate approaches, boy, imagine what we could achieve.
In March of 2016, you are speaking on Illness and Health in a Toxic Society at the 2016 National Council for Behavioral Health Conference. In the description of the topic, you write, “Western practice views people’s health as separate from the social environment, ignoring social determinants of health such as class, gender, economic status, and race. Such factors, in reality, are more important influences on health and longevity than individual predispositions and personal factors such as genes, cholesterol levels, blood pressure and so on.”
With such an array of social and biological factors affecting us, many of which we have no control over, how can we ever find the right formula for long-term health and happiness? What would you recommend to your patients?
John, what I recommend is consciousness. People have to be aware of where their behaviors come from, and what stressors they’ve taken on, what stressors they continue to take on, which of those stressors are avoidable, which of those stressors are not avoidable and you just have to adjust to them, but they have to do so consciously. In a society that stresses people so much, there are no individual answers. There is no individual solution.
For example, the fact that Native Canadians have so much more mental illness, addiction, alcoholism, autoimmune disease and so on is not out of some individual choice that they make. It’s not just the choices that they make in their lives. It is difficult because they need also to really struggle against the social factors that continue to keep them in states of illness.
Until people manage to change society so society takes a different approach, suffering is going to happen. On a certain level, there is no individual solution, but in terms of what advice I’d give to individual patients, you have to live with the way it is, even as you wish it was otherwise. You can work to make it different, but so long as we are living in the world we are living in, you have to deal with the way the world is. What people need is a lot of awareness, a lot of consciousness so they can identify stressors and eliminate them when they are capable of doing so and find ways of living with them when they can’t. Emotional isolation is a major risk factor for disease, addiction, illness, death and everything else. They have to create conditions in their personal lives that as much as possible counteract the stressors that are caused by the society that they live in, and they need to be conscious and aware in order to do this. This is what I would recommend.
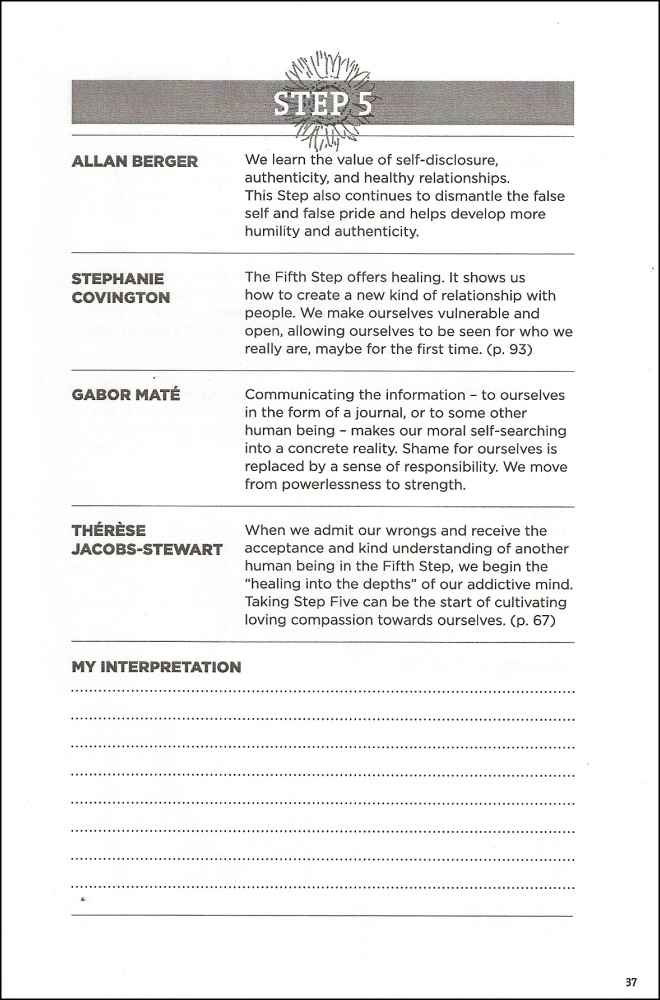
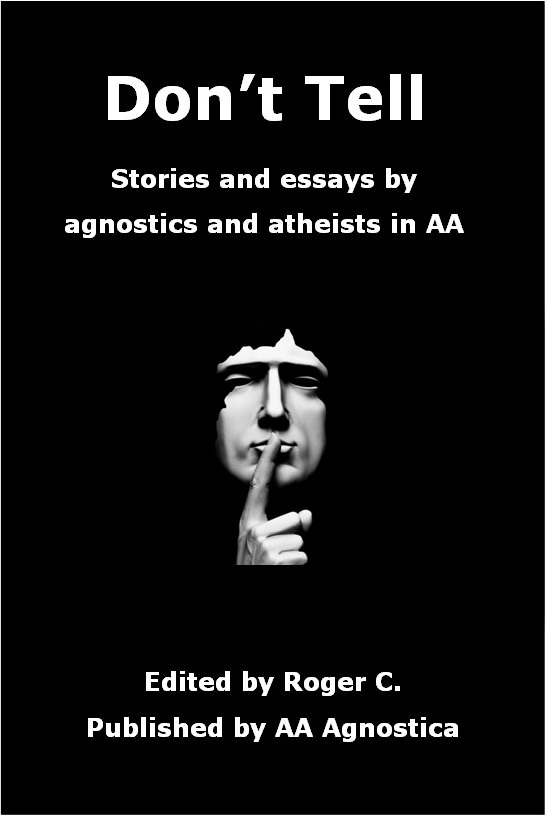
Early on in the above article Dr. Maté says, “I completely appreciate the 12 steps, and I talk about them in my book where I have an appendix on them.”
In 2012, he agreed to have his secular interpretation of the each of the Steps included in The Little Book: A Collection of Alternative 12 Steps. You can see his interpretation of Step 5 in The Little Book here (along with three other interpretations):








One of the leading lights of scientifically-based treatment of addiction which holistically deals with the whole person, body, mind, & spirit, within which the environment, society and culture that the addict is immersed is factored in.
I commented on FaceBook that I believe were Bill Wilson alive today — and perhaps even Dr. Bob, I’ll add — they would deeply respect Gabor Matè and engage in communication with.
Wonderful article. I agree with Dr. Mate 100%. I especially appreciate his view on positive vs. negative thinking vs. just thinking. He is so on pointe with his assessment of the damage of too much positive rosy thinking. We live in a real world made up of both positive and negative. Accept both. Keep up the good work.
Dr. Shaughnessy
Thanks so much for posting this great interview! Without doubt this is among the very best pieces I’ve read. His work on understanding underlying causes and conditions of addiction are spot on in my experience. He truly gets to the root of the problemc like no-one else. I’m confident this would have surely pleased Bill Wilson, Dr. Silkworth and others. A must read for every therapist, as well as 12- steppers!
This is really excellent. Gabor Mate is such a clearheaded thinker.
I have no criticism whatsoever to this piece, which I admit is highly unusual. Mate is just that good. What is left to say about it all is that if Bill Wilson had come to Rockefeller and told him he was putting together a program which focused on the way our society traumatizes people, Rockefeller would have squashed Bill Wilson’s program like a bug.
What Bill did instead was put together a program which helped alcoholics stay sober by finding god. That fell in good soil with Rockefeller and all his buddies.
No challenge to the political system which causes all the stress and trauma.