Psychedelics in Addiction Treatment

Editor’s Note:
For decades, brain chemistry has been a growing field of knowledge on many fronts, including addiction treatment. Early work with psychedelics for addiction treatment in the 1950’s and 60’s – in which Bill Wilson took part – was brutally truncated by the War on Drugs, even though it seemed promising. Now, with so much more known about neurochemistry, it is only logical to revisit them, and the cracks showing up in the War on Drugs makes that possible.
We are not talking about recreational drugs any longer, in this context. It was the uncontrolled social use of psychedelics that caused them to be grouped with narcotics in the first place. And perhaps rightly so, for used without knowledge and care, they can be as dangerous to an individual as fire in the hands of a child. As Dr. Gerald Thomas points out in the article, using these drugs effectively and safely is not a matter of cutting a patient loose on an uncontrolled trip: “When your psyche is cut loose at that level, you need support,” says Thomas. “What is the prep for that? What prepares you to do this? What’s the follow-up protocol?” This is an important focus to current research: not just stopping the physical addiction, but dealing with the underlying psycho-social problems as well.
Some still find new addiction treatments with psychedelics very controversial, but I think it’s only because people haven’t been paying sufficient attention. You know, when James Watt did his thing it was “steam engine time”, and when Einstein did his thing, it was “relativity time”. Now it seems to be “psycho-pharmacological addiction treatment time” – and, importantly, with the understanding that social and psychological supports are necessary as well. The very promising findings so far make this relevant to every addict everywhere, whether she is up to date on the news or not. There may never be a “one treatment cure” for addiction, but as the article shows, there is promise of a vast improvement over the current collection of methods that, frankly, don’t work very well for most people.
Years ago Bill Wilson wrote: “Research has already come up with significant and helpful findings. And research will do far more.” Unfortunately AA has not shown any interest in science or research. It has a Literature Committee but not a Science Committee. While the fellowship will always be important in addressing an alcoholic’s social needs, a real science of neurochemistry may very well make the necessary “psychic change” needed in recovery much more accessible than it was, say, in the 1930s.
Chris G.
The “turn on, tune in and drop out” age of psychedelics created a collective burnout, but these controversial drugs may be the answer for this era’s addiction and depression epidemic.
By Viia Beaumanis
Published in Zoomer Magazine, 23 November 2016
Copyright ZoomerMedia Limited
An aviation prodigy, who first flew in a friend’s plane at 13 and wanted to be a pilot after seeing Top Gun, C. J. Hardin signed up for active duty at 21, the day the Twin Towers fell. Pulling multiple tours in Iraq and Afghanistan as a sergeant in the 101st Airborne Division, Hardin was diagnosed with Post-Traumatic Stress Disorder (PTSD) after his second deployment. Army doctors issued a stack of prescriptions: antidepressants, drugs to keep him alert, sleeping pills for insomnia, blood pressure meds to prevent the nightmares.
“When I left the military in 2010 and returned to the States, I quit all the meds,” says Hardin, now 36 and living in Charleston, S.C. “But I wasn’t functioning. I drank a bottle of rum and half a dozen beers every day, smoked a ton of pot. I bought a camper and lived on my family’s land. I wouldn’t leave the house. I was unemployable.”
In 2013, Hardin learned about MDMA therapy (MDMA is also known as the “love drug” Ecstasy) and signed up. “I quit pot, submitted a clean drug test and got through a lot of interviews and examinations before I was admitted into the program. Then I had three MDMA sessions a month apart. After the first one, there was a major difference, like a giant weight had been lifted off my back. MDMA was like a blanket that wrapped around me and allowed me to talk about things I’d never been able to talk about with anybody. Without MDMA as a catalyst, I’d never have been as open. By the third session, I felt like I was wrapping it all up and closing the book.” It’s not a magic pill, he adds. “You need the PhD therapist with a lot of experience in psychedelics to go with it.”
Clinical studies treating veterans for PTSD with MDMA report that just three months of care – weekly psychotherapy enhanced by three day-long MDMA-assisted sessions – offers a more than extraordinary 80 per cent success rate. And the effects are lasting: researchers monitored patients, who included firefighters, police officers and survivors of childhood sexual abuse as well as veterans, over a three-and-a-half-year span.
“The veteran suicides in America are a national tragedy: 22 every day. MDMA shows extremely positive results while no other medications – anti-depressants like Zoloft and Paxil – work well,” explains Rick Doblin who founded the Multidisciplinary Association for Psychedelic Studies (MAPS) in 1986 and pioneered the research in conjunction with clinical scientists in Canada, the US, Switzerland, Spain and Israel. Pending final trials, MDMA looks slated to become a federally approved prescription drug, legal for therapeutic use, in 2021.
“When I started MAPS, people thought it would never result in anything,” Doblin says of his California-based research and educational foundation that’s currently supporting global studies in MDMA, LSD, ibogaine (the psychedelic extract of an African rainforest shrub) and ayahuasca (a hallucinogenic brew used for centuries as a sacrament by the medicine people of the Amazon) – all of which are proving remarkably effective in healing a broad array of behavioural and mental disorders. “It’s turned around so much over the last few years that now leading institutions are reaching out to us. This week, I had emails from Johns Hopkins and Harvard about organizing new studies. I just got off the phone about a meeting with Stanford researchers. Mexico hosted a Global Ibogaine Conference last March. I recently spoke at McGill. The cultural shift is happening and presenting an opening for the research.”
Johns Hopkins has already documented 80 per cent success rates in ongoing trials curing nicotine addiction with psilocybin-enhanced therapy (the active ingredient in magic mushrooms). LSD-assisted end-of-life counselling to assuage fear of death is showing very positive results in research conducted by the Swiss. Having tested MDMA on anxiety as well as PTSD and psilocybin for cluster headaches with great success, Harvard researchers are ready to launch an ibogaine study. The Heffter Research Institute, a Santa Fe organization that focuses exclusively on psilocybin, is backing clinical trials on that substance’s effects on everything from alcohol addiction (University of New Mexico) and OCD (University of Arizona) to anxiety and depression (UCLA and Johns Hopkins).
“Ketamine is considered the most important break-through for major depression in decades,” continues Doblin of a surgical sedative that was adopted as the party drug Special K. “Taken at 1/10th of the anaesthetic dose, it’s a fast-acting antidepressant. The effects are instant and last a week.” Unlike standard meds such as Prozac, which are aimed at serotonin receptors and take two to eight weeks to kick in, ketamine targets neurotransmitters and boosts synaptic proteins, offering significant results in two hours.
“For severe opiate addiction, I’d recommend ibogaine for withdrawal, then ayahuasca to process the underlying issues,” says Dr. Gabor Maté, a Vancouver physician long admired for his tireless work with inner-city addicts. “Ibogaine stops the Withdrawal completely. You can be on heroin for 20 years and walk out not physically addicted. It also affects the endorphin circuits, inducing a feeling of calm that lasts about three months.”
Detox symptoms eliminated with a single dose of ibogaine, patients are then guided through a few sessions of ayahuasca-assisted counselling. Maté takes the view that compulsions trace back to emotional trauma, and that ayahuasca is a doorway to resolving psychological problems at a deep level. Sometimes referred to as the spirit molecule for its transcendent qualities, ayahuasca’s active ingredient is DMT, which affects several neurochemicals, including serotonin, and some assert allows patients to access the unconscious mind. Combined with psychotherapy, it can untangle the pathology that fuels addiction and other issues, its advocates claim, helping people to understand why they engage in self-destructive patterns and to make healthier choices.

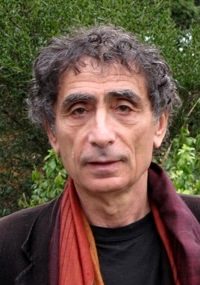
Dr. Gerald Thomas, collaborating research scientist for the Centre for Addictions Research of British Columbia, at the University of Victoria.
Designing a study on the long-term effectiveness of ayahuasca on addiction for MAPS-supported research in 2010, Dr. Gerald Thomas, collaborating scientist for the Centre for Addictions Research of BC, combined Western psychiatric techniques and South American healing practices. Observing ayahuasca-assisted therapy led by Maté in a ritual setting with six months of follow up, Thomas reported “a significant reduction in chronic cocaine and nicotine use along with an overall increase in hopefulness, empowerment and sense of meaning in life. But no reduction with alcohol or – without the ibogaine pretreatment – opiates.”
“Fundamentally, ayahuasca allows people to gain access to, then resolve deep-rooted emotional trauma,” explains Thomas, which, in turn, reduces compulsive behaviour, harmful thought patterns and substance abuse. Though he cautions that ayahuasca, “a concentrated source of truth,” can be intense and should only be administered within an appropriate therapeutic context. “When your psyche is cut loose at that level, you need support,” says Thomas. “What is the prep for that? What prepares you to do this? What’s the follow-up protocol? That’s what I’m interested in.” Queried as to whether ayahuasca should be prescribed as a curative by licensed physicians, he replies, “That’s already happening, along with LSD and psilocybin referrals. The problem is people flying off to retreats in the Peruvian jungle where they have experiences they’re unequipped for.”
At the same time, regulation in North America is all over the map. Though granted an exception for religious use by Latin-American practitioners in both Canada and the States, ayahuasca is not authorized for therapeutic purposes in either country. In 2011, Maté received attention for his progressive addiction therapy, including positive profiles in the Globe and Mail and on CBC’s The Nature of Things, followed by a cease-and-desist letter from the government. Conversely, ibogaine is legal in Canada with clinics specializing in week-long detox therapy for a $6,000 fee not covered by anyone’s health plan. On the other hand, ketamine is not licensed as a treatment for mood disorders in this country but is perfectly legal in the U.S.; chronically depressed Canadians hop the border to access clinics that offer a series of six intravenous sessions – for US $3,000.
“If we were legally allowed to offer these therapies,” says Maté who, in 2009, frustrated with the dismal results of traditional treatments began exploring psychedelic remedies, “we could save millions of people.”
And millions of dollars – an angle that has encouraged governments to take notice. In Ontario alone, one in eight deaths between 25 and 34 is linked to opioid use. Addicts relapse repeatedly despite multiple stints in rehab. Every year, nearly 4,000 Canadians commit suicide – the fourth leading cause of premature death worldwide – with 230,000 adult Ontarians “seriously” considering it annually. Men are more successful; women try more often; over half are 45 and older. According to a 2012 Statistics Canada report, one in three Canadians suffers a mental or substance abuse disorder in their lifetime.
However, unlike MDMA, which can be factory-produced in pill form, an exact dose every time, most psychedelics swim in choppier approval waters. More hallucinogenic LSD and psilocybin are freighted with cultural baggage. Ibogaine is an immobilizing 24- to 48-hour trip. Ayahuasca – an organic extract that varies in strength and is administered in a ceremonial environment that proponents argue is crucial to its efficacy – is hard to evaluate using conventional scientific protocols.
“How do you conduct a double-blind clinical study in a ritual setting where context – environment, guidance, intention – is as key to the treatment as the substance itself?” asks Maté. “We need to get past this nonsense where ayahuasca studies are required to apply Western medical models to a modality developed under a different, unique, ancient practice. It’s not possible to strictly quantify ayahuasca. We should look to the results of countries that have been using it for centuries.”
On which note, let’s rewind.
A stop on the Canadian Pacific Railway noted only for its grain production, Weyburn, Sask., was the last place one would suspect as a hotbed of unconventional activity. Yet here in the pristine wheat fields of central Canada, researchers at Weyburn Hospital began experimenting with “psychedelic” drugs in the early 1950s. Led by Dr. Humphry Osmond, the British psychiatrist who coined the term, physicians investigating the deterring effects of LSD and mescaline (the active ingredient in peyote) on alcohol addiction were soon claiming a 50 per cent success rate, which far outstripped the orthodox approach. With doctors and researchers in America, Europe and the UK. reporting similar findings across a variety of psychological and substance abuse problems, reports of a “miracle cure” began circulating throughout the international medical community, the venerable Time magazine declaring LSD “an invaluable weapon to psychiatrists” in 1955.
Then it went wide, kicking off the Age of Aquarius, the era’s tag line – turn on, tune in, drop out – provided to Timothy Leary by Marshall McLuhan, Canada’s renowned philosopher of communication theory, over lunch at New York’s Park Plaza hotel. The medium is the message: by decade’s end, with Richard Nixon denouncing Leary as “the most dangerous man in America,” LSD had been recast as a street drug that was driving the kids insane. Declared a Schedule I Substance and slapped with a global ban, that was that. Psychedelics of any kind were outlawed even for therapeutic use or research – much to the dismay of psychiatrists and scientists worldwide who had been recording startlingly positive results in clinical settings.

Dr. Deborah Mash professor of neurology and molecular and cellular pharmacology at the University of Miami.
It wasn’t until the early ’90s that cracks began appearing in the medical moratorium. In one example, Dr. Deborah Mash, professor of neurology and molecular and cellular pharmacology at the University of Miami, came across the ibogaine research of Stanley Glick. Former head of the department of neuropharmacology and neuroscience at Albany Medical College, Glick had hooked rats on morphine dispensed via self-serve tubes, then established that they voluntarily decreased the self-administration of the drug after a single dose of ibogaine.
Keen to analyze its potential on humans, Mash obtained FDA approval to run clinical trials, then applied for government funding, but her proposals were repeatedly declined. Appealing to pharmaceutical companies, a customary source of progressive drug research subsidies, proved another dead end. The naturally occurring extract of a West African plant that patients took just once, ibogaine offered no patent and little potential profit to Big Pharma. Quite the reverse; it presented a cure that cut into the massive revenues from methadone, the addictive, commercially produced heroin substitute doled out to millions by government-sanctioned clinics.
Denied funding, Mash opened a private research centre on St. Kitts in 1996. Collating data on 300 crack and heroin addicts detoxed with ibogaine, she found it 98 per cent effective in eradicating painful withdrawal symptoms. Following treatment her patients reported no cravings; 70 per cent went into remission for several months. Half were still clean a year later.
MAPS has also verified positive results with ibogaine. A 2005 University of California San Francisco study showed that alcohol-addicted lab mice sharply reduced consumption after taking ibogaine, then exhibited an increased propensity for staying sober. The key to ibogaine’s impact, researchers concluded in The Journal of Neuroscience, was its ability to boost a brain protein linked to pleasure and reward.
Let’s compare those results to traditional rehab.
Facilities are uniformly modelled on the 12-step program pioneered by Alcoholics Anonymous, an organization with a “success” rate of less than 10 per cent. A review by Cochrane, a leading scientific research organization, determined that no addiction study conducted between 1966 and 2005 “unequivocally demonstrated the effectiveness of AA or TSF [12-step facilitation] approaches for reducing dependence.”
“There’s absolutely no evidence that the treatment works,” says Gabrielle Glaser, an award-winning journalist who writes extensively on addiction and mental health. “Twelve-step programs are not based in science, and rehabs are unregulated. Some have financing departments to help you take out a second mortgage to cover the bill. Families are desperate; they want to believe in the cures being promised. It’s shameful to discuss, so people don’t, and the system perpetuates itself.”
In the meantime, a 2011 government report disclosed that Nova Scotia spends $243 million on alcohol addiction-related issues (treatment, hospital stays, impaired driving, law enforcement, lost productivity) every year – $19 million more than the province’s revenue from the sale of alcohol. The annual cost of alcohol addiction is near $5 billion in Ontario, which spends another $156 million funding methadone for its roughly 50,000 opioid addicts. In 2014, B.C. spent $44 million on methadone. America, where heroin use has more than doubled between 2007 and 2012 – a national pandemic – devotes $24 billion annually to substance abuse.
So, addiction is intransigent, expensive to the taxpayer and enjoys a huge spike when mental health issues are at play; traditional rehab scores a D; prohibition doesn’t work; and emotionally unbalanced individuals are more inclined to chronic substance abuse and less likely to be employed and thus on social assistance. That’s the cycle we’ve been stuck in for decades. What’s needed, argue reformist scientists and researchers, is a raft of government-approved – and funded – studies in the emerging field of psychedelic medicine.
Growing up in Toronto, Lisa, now 50, was drinking at 11, into cocaine by 15 and had alighted on heroin as her drug of choice at 18. Charged with trafficking when she was 24, the courts offered her prison or methadone, and she spent the next two decades on drug replacement therapy. “But methadone does nothing to curb addiction,” says Lisa, who augmented her “treatment” with crack cocaine, cooking it with vinegar so she could inject it. A prostitute and drug mule, in and out of a dozen rehabs by 39, her body shut down. Weighing 80 pounds, covered in abscesses, suffering from hepatitis C, her hair falling out, she had such severe pancreatitis it was misdiagnosed as cancer.
Dr. Gabor Maté, author of In The Realm of Hungry Ghosts.
Giving up everything but methadone, Lisa gradually tapered off the drug, which triggered opiate withdrawal psychosis. Enduring frightening mental breaks, she bounced from doctor to doctor.
None could help – until she came across In the Realm of Hungry Ghosts, Maté’s award-winning book on the neurobiological roots of addiction, and set up a meeting. “We spoke for hours. At the end, he said: ‘It won’t be easy, but I have a way for you to get clean.”
Lisa was admitted to Crossroads Treatment Centre, a detox clinic in Mexico, where ibogaine facilities have become a thriving cottage industry. Going through the treatment twice, Lisa spent six weeks at the clinic. “I was hooked up to an EKG machine to monitor my heart; a nurse on one side of the bed and a paramedic on the other. Everyone’s experience is different. I envisioned Pac-Man-like creatures rushing through my veins, eating everything up. It would get very intense, but at the same time, I felt the plant medicine was saying to me: “We’re here to clean you up, to wake you up.” Afterward, the urge was gone. “But I came home pretty weak, and a lot of emotions came up. Twenty years numbed on methadone, there were a lot of flashbacks. That’s when Dr. Maté suggested ayahuasca to clear the trauma, and I went to a retreat. It’s cleared my spirit, made me lighter, given me a sense of purity. It’s like a divinity is working through you. My mother did it too – she’s in her 70’s – and it was life-changing for her as well. I finally feel like I have something to contribute to this world. Now I work with female addicts. For the really hard cases, I refer them to Dr. Maté. I owe my life to him.”
While many are skeptical about avant-garde wonder cures or trepidatious about psychedelics in particular, people doing innovative work that challenges the status quo is what pushes science forward. Spending billions a year on treatments proven as expensive as they are ineffective is a waste of tax dollars that could be more shrewdly disbursed researching new protocols that are proving adept and efficient and, thus, would be less costly to cover. Yet, with numerous psychedelic clinical trials being conducted internationally by prestigious institutions over the last decade, Health Canada has authorized exactly one: a 2014-2016 Vancouver study on MDMA-assisted psychotherapy for PTSD that just concluded with an 80 per cent success rate.
“In comparison to other countries, the Canadians were unbelievably difficult,” recalls Doblin of prolonged efforts by MAPS to organize the study, which the Harper government took five years to approve. “Then, we had to install bulletproof glass, motion detectors, and an alarm system. All to guard a small safe holding a few grams of MDMA in a pharmacy that was well stocked with far more dangerous and lucrative drugs.” This is a ridiculous stance that Doblin is optimistic will improve under the Trudeau administration. “I just spoke to a colleague who works for the B.C. Ministry of Health and does a lot of drug policy work, and what he said was: ‘We’re back!’”
Determined to bring ibogaine treatment to more people, Mash is now working with private funding to isolate noribogaine, the substance created by ibogaine in the liver that inhibits cravings, to create a more widely acceptable version of the treatment without its hallucinogenic effects. Rick Doblin of MAPS agrees that stripping ibogaine of its psychedelic properties will make it more palatable to approval boards and drug manufacturers but suggests that removing its “insightful” angle will decrease its effectiveness. “The psychological effect, as much as the physiological aspect, is beneficial.” While MAPS studies have found ibogaine for addiction very affirmative, Doblin says, “the one-dose miracle-cure model is unrealistic,” as curing hardcore users of the physical dependence doesn’t free them of the emotional pathology. The winning approach is a holistic one that combines ibogaine with counselling and follow-up care that addresses triggers. Noting that it caused fewer deaths than methadone, New Zealand reclassified ibogaine as a prescription medicine for opiate addiction in 2009.
“The truth is, we don’t have a medical system, we have a pharma delivery system,” says Thomas, “aimed at treating the symptom, not providing the cure, with pharmaceuticals irresponsibly administered and over-prescribed. It’s very ineffective. But there’s also a lack of cultural context for these emerging substances and qualitative differences between them that we need to consider. We have to upload these new drugs onto Western society with thoughtfulness. Do it right and carefully.”
“Five years away,” predicts Doblin of when psychedelics, starting with MDMA, could become legal for therapeutic use. Viewing Nancy Reagan’s passing as the end of an era in more ways than one, Doblin concludes: “I’m looking forward to a time when, instead of Just Say No, we can just say thank you.”
This is the third article on AA Agnostica specifically about psychedelics and their use in the treatment of alcoholism and addiction. The first explored AA co-founder Bill Wilson’s use and interest in psychedelics, Bill Wilson’s Experience With LSD (May 10, 2015), while the second was about Ayahuasca and Addiction (August 30, 2015).









Interesting. I have worries, however. Such compounds may be more suitable for use in rehabs than outpatient since outpatient may involve increased highway risks and presupposes effective control of prescriptions by practitioners. At least in some states (Florida has been mentioned) “prescriptions” in large amounts have been available at street front “pain clinics”. The drugs are then transported to other states and sold on the street at substantial markups. Government regulation has not always been effective to control practitioners who over prescribe either for profit or to spend minimal time with patients, treating them symptomatically rather then determining the cause.
We were talking about LSD for depression in my Smart Recovery and LifeRing meetings. I would do it under doctors supervision in a heartbeat to see if it would help my depression. I have not and never will get on anti depressants but I would try LSD just like Bill W did. It seemed to help him.
Now and then I raise the topic of psychedelic drugs in AA meetings or among my sober friends. It is not a well received topic. I regard the first two times I took LSD to be among the most important experiences of my life. I sincerely believe that there might be real benefit to me of taking such a drug again. However, ultimately, I have come to the realization that I can’t do that and still claim to be someone who doesn’t use drugs. Somewhat to my surprise I find remaining totally abstinent more important than yet another drug induced experience. That has no bearing, however, on the importance of the research results you have reported here. I have found again and again that AA is, for the most, part openly hostile to discussions regarding modern research into the nature and treatment of addiction. Lip service is given to the “disease model of alcoholism” but minds are closed to relevant scientific investigations and factually supported conclusions. Perhaps this article delivered in this venue will find open minds. I hope so.
This is such an important article, relating current evidence-based research for the effective treatment of addiction — thank you, Roger.
The efficacious use of such plant medicines was demonstrated in a number of studies during the 1950s. These results recently have been replicated under much more stringent and reliable research protocols, demonstrating that plant medicines deal with the “root causes and conditions” of addiction much more efficaciously than 12-step treatment regiments.
However, I fear with the upcoming Trumplandia administration in the US government, such advances will likely be considered as witchcraft, especially if they cut substantially into the huge profits of Big Pharma.
A pity – one step forward, ten steps backwards…
AA’s seeming lack of interest in science and ongoing research is troubling. I am active in SMART Recovery and left AA (mainstream and secular) in the rear view mirror in part because of this “ignorance is bliss” paradigm that seems to pervade AA from the NYC office to the local basement meeting. Psychedelics, The Sinclair Method, Harm Reduction/Moderation, Cognitive Behavioral Therapy and so many other approaches have worked for so many and are rooted in peer reviewed research. That is not to say that AA has not worked for millions – it is quite simply not the only way. It is exciting that so much research into alternative treatments is underway.
As someone who attends N.A. for the social aspects and support, I’m constantly amazed that these 12 step programs with their dismal success rates don’t modify and/or update their formula! It’s archaic. Back in the late 30’s when A.A. was in it’s infancy, it was believed that addiction/alcoholism was a moral failing and/or a lack of will power. But today after many decades of research, we now know that’s just not true. Yet they continue with their grossly outdated 12 steps!
Roger thanks for this.
Important stuff. Living in the Emerald Triangle I’m very much aware of the disparity between big pharma and government on the one side, and, well, everyone else trying to find better and more reasonable solutions on the other.
And now, though unrelated, but since we don’t at present have a blog or anything like that, please allow me to briefly introduce a book I have read this last week (rather than wait until I have occasion to write a review):
Lance Dodes: The Sober Truth.
The first half of the book he discusses scientific method, and also goes to great length to discuss from a statistical angle that AA doesn’t really work. There is a lot of good stuff in there, for instance about compliance effect and concurrence vs causality, but it is also tiresome in passages. In the last half he gets more into the psychology of it all, his primary thesis being that all addictive behavior starts with a sense of overwhelming helplessness. This part of the book I found to be really good to read.
Though he is on a mission to discredit AA there is a lot of good stuff in there, much of what I myself have been thinking and feeling about AA, and he’s not down at the same vendetta level as Orange. Worthwhile read.
A very interesting update and overview of a subject that has been around for 60 years or more.
As to the efficacy of these substances the only touchstone I have is my own use of LSD many years ago between late 1967 and mid 1972. My recollection is that this drug was used to get totally blasted and that the insights, if any, were minor when compared to the great good times being had in those days just getting stoned.
Sadly, I also recall the State Mental Hospital that was very near my College that ended up having a whole floor that was devoted to psychedelic casualties of one sort or another.
Somehow, having seen a number of these “tripped out” cases, I had made a pact with myself that if I ever got frightened using acid that I would stop at once. When that day came in the spring of 72′ I put that stuff down and never used it again. This allowed me to get down to a proper relationship with my true drug of choice, Mr. Jack Daniels, who had me in a firm grip until January of 1987 when I finally put plug in it as the old “Old Timers” used to say.
Obviously, in my case, an extensive exposure to these mind altering substances didn’t cure me of any propensity I had to addictive behavior much less give me any access to a so-called “spiritual experience” that may have had a positive effect.
This is purely anecdotal and only applicable to myself in any clinical sense but it is the genuine experience of at least one alcoholic that may be shared by others.
Having said all that I don’t hold a medical degree, am not a psychopharmacologic expert or psychologist and have no expertise with clinical trials.
This research should go on and everyone (my skeptical self included) should have an open mind to the real science, clinical trials, and true peer reviewed studies as they become available.
We should be aware though that these drugs are “heap big medicine” that could prove problematic for the alcoholic/addict if misused. I, for one, would not jeopardize my nearly 30 years of success with the admittedly limited AA program by even thinking of using such things myself.
For people struggling with chronic relapse there may be a place for these things. For others, with other medical conditions such as depression,mania, OCD, etc. there could well be other complications.
Before running to something “new” that has the potential of doing further harm the science has to be rock solid. I don’t see such a foundation here and elsewhere so (as it was in Bill W”s time) these approaches remain “experimental”. It might be wise to look deeper into the reasons for why that is the case.
Let’s not forget the Native American Church, in which the hallucinogenic peyote is a sacrament. While the NAC is a syncrenistic religion, mixing some elements of Christianity and traditional indigenous ways, one of its tenets is abstinence from alcohol. I know men who were once bad alcoholics on the streets of Denver, Oklahoma City, and Seattle. They have been sober for a long time in the NAC. They are leaders in their communities. Yet, some people in AA say that they aren’t sober because of the use of peyote.
I strongly disagree with the premises of this article, that drugs and therapy are needed to successfully stop drinking or smoking. The overall approach is what James R. Milam called “psychogenic” – the idea that alcoholism is merely a symptom of underlying psychological problems. Milam’s “biogenic” approach holds that alcoholism is a physical addiction to the drug, ethyl alcohol; that alcoholism causes character defects or psychological problems, rather than the other way around; and that recovery requires total abstinence.
It is insidiously wrong to judge AA as a form of “treatment”. The AA Preamble concisely and cogently describes what AA is and is not. AA is a Fellowship of recovering alcoholics, who share experience, strength and hope with each other in order to get and stay sober and lead good lives in sobriety. The 24-Hour Plan, not Bill W.’s Steps, is the heart of AA.
This article approvingly cites Gabrielle Glaser as an authority on alcoholism. She is not. I suggest reading some of the one-star reviews of her book, including my own review, “Dishonest and Harmful.”
John L: The article does not claim that drug therapy is always necessary for recovery from addiction. It claims that drug therapy can sometimes bring about positive results. Whether you agree or not is, of course, your choice. Whether this observation is true or not is actually a matter of independently verifiable fact. The evidence collected by many careful scientific investigators appears to overwhelmingly confirm the utility of drug therapy in treating addiction in many cases. This does qualify this approach a treatment – which as you accurately point out AA is not. This is good news and need not threaten those of us who have recovered from addiction without the use of drug therapy. The more avenues to recovery the better. Right? Bill W himself presiently pointed out that “one day science may discover” ways to treat alcoholism. I imagine he would approve.
I believe that all areas of addiction, whether alcohol, opiod, ad nauseum must be investigated scientifically in response to our completely failed war on drugs. This is a public health issue, not criminal justice. We need treatment upon request not more mass incarations. Portugal has lead the way with total decriminalization with remarkable success.